Dental sterilization is the process of eliminating all forms of microbial life from dental instruments and equipment. It is a critical component of ensuring patient safety and preventing the transmission of infections and diseases. In this blog post, we will discuss the importance of dental sterilization practices, the risks of inadequate sterilization, the key components of effective sterilization processes, the regulatory guidelines and standards, and the role of education and training for dental staff. We will also highlight the growth potential of the globaldental sterilization market size, which is expected to grow in the forecast period of 2024-2032 at a CAGR of 5.5%.
Understanding Dental Sterilization
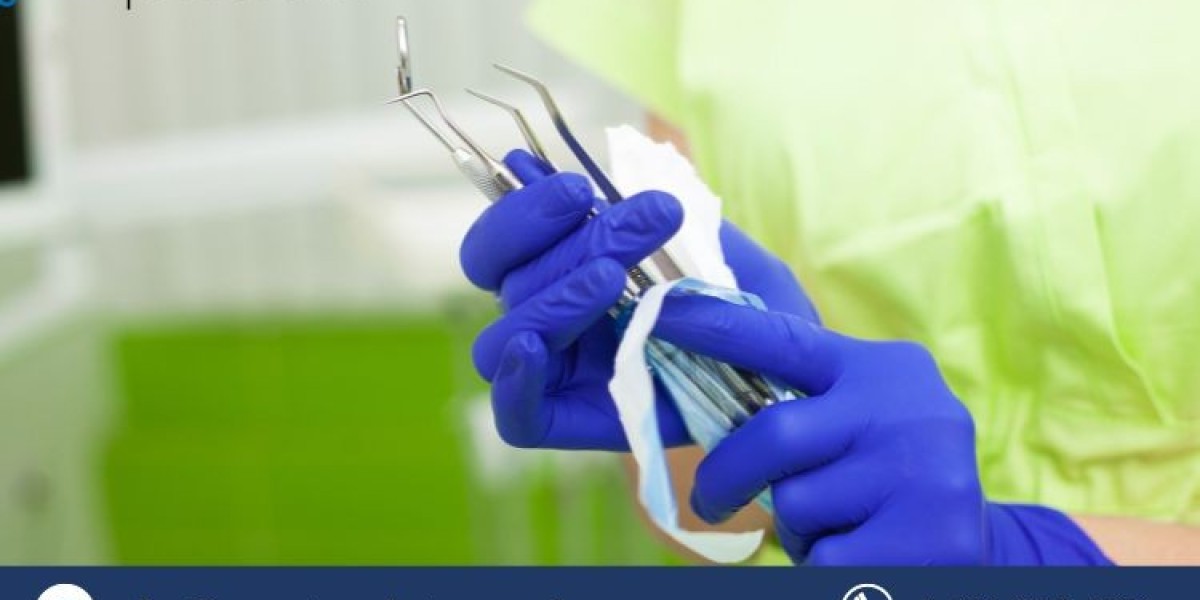
Sterilization is the highest level of disinfection that can be achieved for dental instruments and equipment. It involves the complete destruction of all microorganisms, including bacteria, viruses, fungi, and spores. Sterilization is essential for preventing the transmission of infections and diseases that can occur through direct or indirect contact with contaminated dental instruments. Some of the common infections and diseases that can be transmitted through dental instruments include hepatitis B and C, HIV, tuberculosis, herpes, and syphilis.
Risks of Inadequate Sterilization
Improper sterilization practices can pose serious risks for patient health and safety. Contaminated dental instruments can introduce harmful microorganisms into the oral cavity, bloodstream, or other tissues of the patient, causing infections and diseases that can range from mild to life-threatening. Inadequate sterilization can also compromise the quality and effectiveness of dental treatments and procedures, leading to poor outcomes and complications. Moreover, improper sterilization can expose dental professionals to the risk of occupational infections and diseases, as well as legal and ethical liabilities.
Key Components of Effective Sterilization Practices
Effective sterilization practices require a systematic approach that involves several steps and components. These include:
- Pre-sterilization cleaning: This involves the removal of organic matter and debris from dental instruments and equipment using manual or mechanical methods, such as scrubbing, rinsing, and ultrasonic cleaning. Cleaning is a prerequisite for sterilization, as it reduces the bioburden and enhances the penetration of the sterilizing agent.
- Packaging and wrapping: This involves the placement of dental instruments and equipment in appropriate containers or wraps that protect them from contamination and maintain their sterility until use. Packaging and wrapping materials should be compatible with the sterilization method and should allow the sterilizing agent to reach all surfaces of the instruments and equipment.
- Sterilization methods: There are different methods of sterilization that can be used for dental instruments and equipment, depending on their type, material, and intended use. The most common methods are steam autoclaving, chemical sterilization, and dry heat sterilization. Steam autoclaving uses pressurized steam at high temperatures to kill microorganisms. Chemical sterilization uses liquid or gaseous chemicals, such as ethylene oxide, hydrogen peroxide, or glutaraldehyde, to destroy microorganisms. Dry heat sterilization uses hot air at high temperatures to kill microorganisms.
- Monitoring and validation: This involves the regular testing and verification of the sterilization processes to ensure their effectiveness and reliability. Monitoring and validation can be done using physical, chemical, or biological indicators. Physical indicators include temperature, pressure, and time measurements. Chemical indicators include color-changing strips or tapes that indicate the exposure to the sterilizing agent. Biological indicators include spore tests that use living microorganisms to challenge the sterilization process.
Regulatory Guidelines and Standards
Dental sterilization practices are governed by various regulatory agencies and guidelines that aim to ensure the safety and quality of dental care. Some of the major regulatory agencies and guidelines include:
- The Centers for Disease Control and Prevention (CDC): The CDC provides recommendations and guidelines for infection prevention and control in dental settings, including sterilization practices. The CDC guidelines cover topics such as hand hygiene, personal protective equipment, pre-sterilization cleaning, packaging and wrapping, sterilization methods, monitoring and validation, storage and handling, and quality assurance.
- The Food and Drug Administration (FDA): The FDA regulates the safety and effectiveness of medical devices, including dental instruments and equipment, and their sterilization processes. The FDA requires manufacturers to provide instructions for use, labeling, and validation data for their products. The FDA also inspects and enforces compliance with its regulations.
- The Organization for Safety, Asepsis and Prevention (OSAP): The OSAP is a non-profit organization that promotes education and research on infection prevention and control in dentistry. The OSAP provides resources, training, and certification for dental professionals on sterilization practices and other infection prevention and control topics.
Educating Dental Staff
One of the key factors for ensuring effective sterilization practices is the education and training of dental professionals. Dental staff should be knowledgeable and competent in the principles and procedures of sterilization, as well as the risks and consequences of inadequate sterilization. Dental staff should also be aware of the regulatory guidelines and standards that apply to their practice and comply with them. Some of the tips for implementing effective education and training programs for dental staff include:
- Providing initial and periodic training on sterilization practices and infection prevention and control topics.
- Using a variety of methods and formats, such as lectures, demonstrations, videos, manuals, and online courses.
- Evaluating the learning outcomes and feedback of the trainees and providing reinforcement and remediation as needed.
- Creating a culture of safety and quality that encourages adherence to sterilization protocols and continuous improvement.
Dental sterilization practices are vital for ensuring patient safety and preventing the spread of infections and diseases. Dental professionals should follow strict sterilization protocols, monitor and validate their sterilization processes, adhere to regulatory guidelines and standards, and educate and train their staff on sterilization practices. By doing so, they can enhance the quality and effectiveness of their dental care and contribute to the growth of the global dental sterilization market.